With all the issues surrounding mental health, perhaps none has a bigger impact than parity. But parity also happens to be one of the hardest to understand and hardest to implement. In this episode, we will look at the legislative history of parity, current problems with enforcement, and a new ruling that impacts parity across the country. Insurance parity for behavioral health coverage makes providing behavioral health services possible and it is impossible to improve access without it.
This is Minding Houston, I’m Bill Kelly.
When we talk about parity, we need to talk a little political history. The Houston Chronicle’s Jenny Deam wrote about the situation regarding parity and its roots in federal legislation, and she sums it up nicely:
![]()
“President George W. Bush signed a law requiring any insurance policy that included mental health treatment to be equal in coverage to medical treatment, in an effort to stop the long-standing practice of charging higher co-pays for mental health care, limiting treatment or denying it outright. It was cheered as a triumph for the nation’s millions with mental illness.
The measure was further strengthened in 2010 with the passage of the Affordable Care Act, which extended federal parity requirements to individual and small-group plans and mandated mental health and substance abuse be covered in any plan sold on the federal marketplace or state exchanges.
But the lofty goal of equality has fallen far short of its promise, providers, patients and policy experts say.”
So with federal legislation passed, what’s the problem? Parity is the law of the land, why isn’t it the standard practice of providers? Well, as Ben Franklin once said, “”Justice will not be served until those who are unaffected are as outraged as those who are,” which I think was his way of stirring up those of us who care about behavioral health coverage. Deam’s article continues:
“In fact, certain managed care groups are well known within the Houston behavioral care community of having a “predictably higher rate of denials” and a “higher hassle factor,” says Dr. George Santos, chief medical officer and executive medical director at Houston Behavioral Hospital. “They hide behind statements like, ‘We are not telling you what to do.’ But I have had many instances where these physicians will make specific treatment recommendations regarding medications and doses. They will certainly say a patient no longer needs inpatient care and will deny approval.”
Take Dr. Richard Noel, medical director at IntraCare North, a Houston psychiatric facility. He spends hours each week on the phone arguing with doctors paid by insurance companies who have never seen his patients. He says he now has to prove that medications for inpatient children and teens are being adjusted every few days – often before the drugs have had a chance to work – or insurers will no longer cover a hospital stay. He says he has had issues with nearly all of the major insurance companies.”
What are the consequences when parity for behavioral health isn’t enforced with providers? Well, I would refer to statements made by Dr. William Streusand, an adolescent child psychiatrist at the Texas A&M Health Science center. He testified in front of the House Select Committee on Mental Health on March 22nd and answered the following question from Rep. Greg Bonnen, also a physician:
Bonnen: “You don’t take private insurance in your practice, why is that?”
Streusand: “I don’t have to.”
Bonnen: “Well, okay, could you elaborate on why you wouldn’t have to?”
Streusand: “Yeah, like I said it is a seller’s market.”
While that is true, what else is true, as followers of Minding Houston well know, is Texas has a scarcity of providers. How bad is the situation and how does it affect parity? From the Chronicle article:
“Texas ranks 47th out of 50 states and the District of Columbia in access to mental health care, and 50th in the number of mental health providers with only one for every 1,757 in the state, according to a study by Mental Health America. By contrast, Massachusetts, which ranks first, has one provider for every 248 people.
“They flat out tell me, ‘We don’t take insurance anymore because we have too much trouble getting paid,’ ” says Carrie Stowell, a single mother whose 16-year-old daughter has been diagnosed with bipolar disorder, attention deficit hyperactivity disorder and anxiety. She lives in Conroe and found 10 doctors in a 40-mile radius who treat adolescents, but only one is taking new patients or is in her plan. The wait for an appointment is six months.
Santos also feels the shortage. “It is extremely difficult to recruit a physician willing to work at an inpatient setting because of insurance,” he says.”
Because of poor parity enforcement, Texas finds itself in a situation where access to care is being limited not only to the number of providers but the number of providers that take insurance. Having a “cash only” payment model for behavioral health is a dangerous trend for Texas and can be one of the most limiting factors in the provision of care. Texas has too many people needing services to be a “seller’s market.” It is time to make some changes.
So how can this parity enforcement problem be addressed? Based on his experience as a prosecutor and his observations of the mental health needs of so many in the criminal justice system, Congressman Joe Kennedy III has a plan that he believes can help enforce the parity laws on the books. We talked with the Congressman about his Behavioral Health Coverage & Treatment Act last week:

Bill Kelly and Congressman Joe Kennedy III
Kelly: I’m here today with Congressman Kennedy. Congressman, thank you so much for joining us. In December you filed your Behavioral Health Coverage and Transparency Act and, unlike in Texas where we face large problems due to our large uninsured population, this act primarily goes after folks with insurance looking to access services. What particular aspect really raised this on your radar screen?
Kennedy: So, I’ve been diving into issues around mental health now for a while, since I came into office and, actually, really beforehand. Before I ended up running for office, my first campaign, I was a prosecutor. I cannot tell you how many cases came across my desk from the district courts, lower courts, criminal courts in Massachusetts for folks struggling with either mental illness, substance abuse, drug abuse, or alcoholism and my boss at that point, a Republican DA, said, “Your job is to make sure that person never commits another crime.”
And some folks are bad people and you lock them up for a long time. For others suffering from mental illness or substance abuse, the way you can do that is to treat the underlying condition. It doesn’t matter if you lock them up for three months if they are not able to get treatment for their mental illness or get clean off of a heroin addiction.
So use the tools that you have in your tool kit to help address the underlying concern. As a prosecutor, there are some tools we got; there’s a lot that we don’t and from my perspective trying a bunch of drug cases and working with a lot of drug cases, I became convinced that the way to ensure that those files that were people’s lives on my desk, the way to actually address them much further upstream is to focus on prevention and treatment rather than on prosecution.
The question then becomes how do we make sure there is access to mental health care throughout our society? And as we start peeling back the layers on this, from my perspective on it, there are two main segments. There is the public side of things where folks get their healthcare from the federal government, Medicaid primarily. Medicaid is, of course, the largest payer of mental health care services in the country. Then there is, of course, the private side doing private insurance. We’ve started by looking at the private side marketplace.
What this bill’s focus is to say, look, the combination of mental health parity, which is a simple law that has helped expand coverage, but it’s the combination of mental health parity and the Affordable Care Act that actually said as an essential health benefit in order to participate in these exchanges, you have to actually cover mental health care. So we have the combination of the Mental Health Parity Act, which says we have to treat mental health care like we do physical health care, and then the Affordable Care Act, which says you have to now cover mental health care. That leads to a huge expansion in coverage for states, particularly those who took the Medicaid expansion, which not all states did.
The challenge though is that the marketplaces still are not functioning so we still hear cases all over the country that say “I don’t need to take insurance,” because there are so many people that are in need of care and so few doctors that the doctors are essentially empowered to say “I can cherry pick my clients, I can make sure to get rates that are higher that other insurance companies will reimburse me for and I’ll just be an all-cash doctor.”
The problem with this is that you can’t just create more doctors overnight. So there are systemic issues that are affecting our ability in this country to have patients that are suffering from mental illness to actually access mental health they need. One other step for you: according to one study I saw recently 55% of the counties across our country do not have a single practicing psychiatrist, psychologist or social worker, 55% of the counties across our country!
So when we start talking about trying to get access to care, insurance is an important part to this, but we have to make sure you can actually get a doctor and stay treated. So the bill that we filed is a first step in trying to basically force insurance companies to divulge information around how they are actually covering mental health care. As you know, there are many people that are suffering from mental illness who get their insurance claims denied at a much higher rate than those suffering from typical, physical maladies such as a broken leg or a broken arm. So this bill will hopefully shine a light on some of those practices and force insurance companies to actually make this transition to focus on prevention and treatment, rather than triage at the back end of mental health.
Kelly: And you mention that this bill, it doesn’t put forth any new regulations as much as it focuses on transparency the for given laws that you mentioned with parity and the ACA.
Kennedy: Absolutely. Part of the way we crafted this is to say, look we are not trying to add any additional burden to these insurance companies, but disclose the methodology at which you end up making your decisions and make sure that information is available and digestible to regulators so we can actually start to shine a light on this and ask are things actually going as they should – which case there might be something else that needs to be done – or are they not?
And the idea behind this bill is that if insurance companies can essentially get away with not covering people at the back end when they are in need of mental health care, then there is essentially no reason for them to make the investment they need to actually force the focus of treatment to move up that scale to prevention and treatment rather than just focusing on the back end for folks that end up in a crisis point.
So what we want to do is try to take a step back and say how are we going to address access to mental health care in the system? It needs a full-on continuum of care adjustment. We need the private sector to play a role in that and I think a critical piece to it is by getting insurance companies to not just focus on the back end, the really expensive cases of triage after you’re becoming the victim of mental illness, but to focus on treatment and prevention on the front end. How do we flesh that out? We make sure that you are actually abiding by the terms of the regulation that are already in place.
Kelly: When you talk about the regulations that are already in place, one of the things that make mental health and behavioral health a very bipartisan issue is that people in a very partisan health care landscape, have been really willing to come together. You’ve seen bills move both in the House and the Senate. Do you see your bill possibly being able to hitch onto one of these bills that seem to be making some headway down the track?
Kennedy: Absolutely hope so. This is something that I think Democrats and Republicans agree on, that our mental health system is in crisis. Whether it was folks in Congress that have had similar experiences to me as prosecutors saying this is a real problem, whether you see it in emergency rooms because you have some doctors in Congress, or you are a member in Congress involved in trying to help our access to health care period.
And if you go around even hospitals in Massachusetts it’s one of the things you will hear about in emergency departments is there are a lot of people in their EDs suffering from mental illness. So we hear about this all the time; the question is how do we go about addressing it, again in that full-on continuum of care model? I hope that this legislation will address this, either as a standalone or perhaps as an amendment to one of those other pieces of legislation that we have been working hard on. We have been working with some of our colleagues on it and they have been doing a really good job. There is also a really tricky issue on how to make these reforms across the entire system and some of my colleagues and I are trying to dive into this so hopefully we will get there.
Kelly: Well, thank you, Congressman so much for your time today and for your work on this really important issue that I hope gets the traction that it needs. Like you said, this is a critical first step to ensuring that those with private coverage get the help that they need.
Kennedy. Thank you for your time too, Bill.
As the Congressman mentioned, the largest payer of behavioral health services in the country is Medicaid. And a recent announcement by the Department of Health and Human Services is good news for increasing access.
On March 29th, the Center for Medicare & Medicaid Services (often referred to as CMS) announced the new rule in coordination with President Obama’s visit to the National Rx Drug Abuse and Heroin Summit. From the press release:

” . . . the Centers for Medicare & Medicaid Services (CMS) today finalized a rule to strengthen access to mental health and substance use services for people with Medicaid or Children’s Health Insurance Program (CHIP) coverage, aligning with protections already required of private health plans. The Mental Health Parity and Addiction Equity Act of 2008 generally requires that health insurance plans treat mental health and substance use disorder benefits on equal footing as medical and surgical benefits.
“The Affordable Care Act provided one of the largest expansions of mental health and substance use disorder coverage in a generation,” HHS Secretary Sylvia M. Burwell said. “Today’s rule eliminates a barrier to coverage for the millions of Americans who for too long faced a system that treated behavioral health as an unequal priority. It represents a critical step in our effort to ensure that everyone has access to the care they need.
“This rule will also increase access to evidence-based treatment to help more people get the help they need for their recovery and is critical in our comprehensive approach to addressing the serious opioid epidemic facing our nation.”
“The need to strengthen access to mental health and substance use disorder services is clear,” said Vikki Wachino, Deputy Administrator of CMS and Director of the Center for Medicaid and CHIP Services. “This final rule will help states strengthen care delivery and support low-income individuals in accessing the services and treatment they need to be healthy.”
The protections set forth in this final rule will benefit the over 23 million people enrolled in Medicaid managed care organizations (MCOs), Medicaid alternative benefit plans (ABPs), and CHIP.
A link to the press release and the finalized rule can be found here
Overall, our goal at MHA of Greater Houston has been to make the provision of behavioral healthcare a successful business model. After all, if people want to access services, there needs to be providers available to treat them. Parity can help provide the basic regulatory functions under which providers can be paid in a timely manner for their services. And it is already the law . . .
Parity will continue to be a big issue at the state and national level. We look forward to continuing to work with our elected leaders in Austin and Washington to make sure parity coverage is enforced. Without this level playing field, progress in mental health care access continues to be an uphill battle.
This has been Minding Houston, I’m Bill Kelly.
Music for this Episode: “Hotel Rodeo”, “Quisling”, and Bricolage” by Anitek and “Vacate the Premises” by Deadly Combo





 Bill Kelly: I’m here at the Harris County Psychiatric Center (HCPC) with Steve Glazier. Thank you so much for taking the time to meet with us today. I wanted to first go through and describe the mission and capacity here at HCPC and how it really fits into the behavioral health network of providers here in Houston.
Bill Kelly: I’m here at the Harris County Psychiatric Center (HCPC) with Steve Glazier. Thank you so much for taking the time to meet with us today. I wanted to first go through and describe the mission and capacity here at HCPC and how it really fits into the behavioral health network of providers here in Houston.













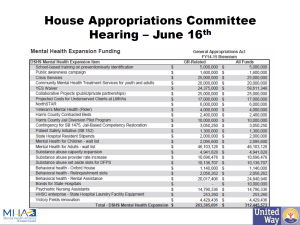
 Rep. Turner: “So in comparison to what we did in the last biennium to this biennium what is the increase or decrease or are the things the same?”
Rep. Turner: “So in comparison to what we did in the last biennium to this biennium what is the increase or decrease or are the things the same?”

 will be key in securing the needed funding for community based programs.
will be key in securing the needed funding for community based programs.





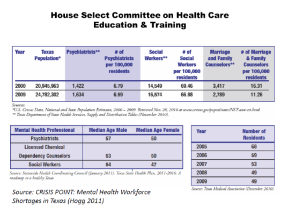
 Unfortunately, things haven’t improved since this report was released in 2011. One of the most respected health care groups in Texas just released a report this January that echoes many of the same concerns. In an interview with
Unfortunately, things haven’t improved since this report was released in 2011. One of the most respected health care groups in Texas just released a report this January that echoes many of the same concerns. In an interview with