Whenever the topic of mental health is discussed, one of the most repeated solutions is to increase capacity, usually in the common phrase, “we need more beds.” But do people really have the facts on what the bed capacity issues are for Harris County, and how does that play into what bed capacity issues face the state? Today, we talk to a leader for Harris County’s inpatient mental health hospital to get very specific on capacity issues.
This is Minding Houston, I’m Bill Kelly
Sgt. Joe Friday should have taught public policy. His “just the facts” line is one of my favorites and carries the objective tone of trying to boil down a problem to its core. So it is in that Dragnet spirit that I hope you don’t mind if we focus on a few graphs and numbers to get the story on capacity for state psychiatric beds.

The Texas Department of State Health Services has often presented the above slide in talking about the number of publicly funded beds available in the Texas State Hospital system. The graph shows two sets of numbers: first, the state hospital psychiatric beds represented with the light blue line, and secondly state funded (or private) psych beds represented by a red line. The black line at the top shows the sum of these two numbers and the overall trend in patient capacity for the state.
What’s apparent from this graph are two things which are important to note when looking at future trends regarding capacity options:
First, the number of state-owned beds has largely flat-lined since 2006, which shows that despite recent investments at the state level, Texas has not increased inpatient capacity for state-owned beds.
Secondly, the number of state-funded, private beds has more than doubled during that same time period, moving close to 20% of the state bed capacity total.
Clearly, the preferred option to increasing state bed capacity has been to buy, rather than build.
However, one number is not included in this data set that is the most important in answering what the real situation is with regards to the capacity of inpatient beds in Texas, and that’s population. Anyone who is living in Texas knows the explosive population growth seen in the past two decades, and in order to get the whole picture, the number of Texans needs to be accounted for in this data.
In a presentation to the Senate Finance Committee on January 15th, Assistant Commissioner Lauren Lacefield Lewis presented the following slide that tracks the total number of state beds to state population, and the numbers are not encouraging:

From the graph, you can see that Texas is currently at the lowest ratio of beds to population since 1994. So in talking about what the psychiatric bed capacity for Texas is, we are starting from the lowest point based on population.
But aside from just the overall population, there’s another factor putting added pressure on the number of psych beds available for Texans: the criminal justice system. In the same presentation to Senate Finance, Mrs. Lewis showed the following slide that confirms a trend that first reached a tipping point in 2014. That trend is that more people are admitted to the Texas State Hospital system through forensic commitments than civil.
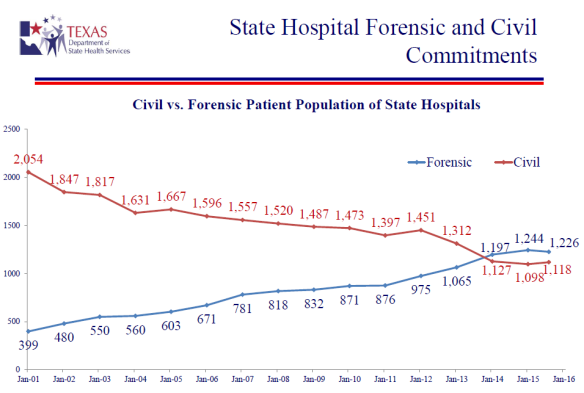
2014 marked the first year that more people entered the state hospital through the criminal justice system (a forensic commitment) than were voluntarily committed (civil commitment). And the trend has continued in 2015 and 2016.
This is a dangerous situation, as the public safety of Texans is now using up resources designed to make sure Texans have access to mental health beds. And the consequences are already showing up in real world situations right here in Harris County.

According to a March 4th Edition of the Houston Chronicle, the number of beds for forensic commitments were supposed to take up a third of the Texas State Hospital system but have instead become a majority.
The case of Shannon Miles, who stands accused of the murder of Harris County Sheriff’s Deputy Darren Goforth last August, has had more than its share of strange twists and turns. The case also has highlighted yet another problem with how the state deals with the mentally ill among us.
To review, Goforth was shot 15 times as he walked to his patrol car at a gas station. Sheriff’s deputies within a day arrested Miles, who has a history of mental illness. On Feb. 9, he was found mentally incompetent to stand trial after experts agreed he suffers from schizophrenia, and he was ordered to Vernon State Mental Hospital in North Texas. There he would receive a 120-day mental evaluation to determine whether so-called competency restoration is possible. As of this writing, he’s still in the Harris County Jail – the state’s largest de facto mental health facility, by the way – because some 60 other Harris County inmates are in line to go to Vernon ahead of him.
In 2012, a Travis County judge ruled that defendants requiring a forensic bed at a state mental hospital couldn’t be made to wait in jail for more than three weeks. Forensic beds are the spaces set aside for defendants, like Miles, who need psychiatric treatment to get well enough to stand trial. As Emily DePrang reported in the Texas Observer in 2014, they’ve had to wait in recent years for an average of six months.
Long waits are still the rule, despite the judge’s ruling, because Texas has less than 2,500 beds at its 10 state mental hospitals; less than a third of those are designated for forensic commitments. The cruel irony is that every bed used by someone from a jail is one less bed available for people who have committed no crime.
The wait list for the state hospital is another example of the lack of access for mental health owing to a capacity for treatment. The bottleneck for violent offenders at the Vernon State Hospital is just one example.

Another example is the overall number of people who are dependent on the public mental health system. Recently, our favorite radio program Houston Matters had me on to talk about the need for crisis clinics while highlighting a new walk-in clinic opened in Meyerland by Memorial Hermann. Houston Public Media has done an extraordinary job when it comes to highlighting mental health, which I think is evident from the questions asked by Houston Public Media’s Craig Cohen. Here’s the part of our interview focusing on the need for services:
Craig Cohen: Bill Kelly, we do tend to think of the need for 24/7 physical health emergency care. Is it something that we tend to forget or not take seriously that there is a need for 24/7 – particularly in the overnight hours – emergency mental health care?
Bill Kelly: Well, I would just point to the overall numbers and then when you look at the gap in coverage and access it really emphasizes the need to invest in them. And according to our State Health and Human Services Commission, we have about half a million Texas adults that suffer from a severe and persistent mental illness. Now severe mental illness results in a serious functional impairment which substantially interferes or limits one or more major life activities. When you add the “persistent” that means that those symptoms have lasted over a year. So if you have half a million adults that breaks down in Harris County to right at 150,000 adults. Now, we know from our Mental Health Needs Council assessment that about 90,000 of that 150,000 have no access to public or private insurance. So the very systems that Memorial Hermann and other partners with the 1115 waiver are trying to build out are badly needed for this group. Like Theresa said, if people do not get the medical services that they need and the mental health care that they need, their safety net all too often is emergency rooms that are already crowded and a system that has a coverage gap or, unfortunately, our criminal justice system.
The capacity question here in Harris County is one that should draw attention. Having such a scarcity of access will place an inordinate demand on existing resources. The relief provided by the expanded footprint of behavioral health from the 1115 Waiver’s DSRIP projects, such as this crisis clinic, should be viewed as vital. We cannot afford to lose these new programs when the waiver expires later in 2016.
Fortunately, we have a resource locally that helps with the inpatient capacity that makes Harris County the envy of other places in Texas. I sat down with Stephen Glazier, Chief Operating Officer of the Harris County Psychiatric Center, or HCPC, to talk about the role his facility plays in helping provide capacity right here in Harris County:
Bill Kelly: I’m here at the Harris County Psychiatric Center (HCPC) with Steve Glazier. Thank you so much for taking the time to meet with us today. I wanted to first go through and describe the mission and capacity here at HCPC and how it really fits into the behavioral health network of providers here in Houston.
Steve Glazier: So HCPC is primarily a short-term acute care psychiatric hospital. We do have a few units that are designed for patients that stay a little bit longer, three or four or five weeks, but the majority of beds are short term acute care which means the patients stay roughly seven to eight days. We are a 276 bed hospital. Currently, we are renovating units; we are going to have our 30th birthday in the fall and 30 years of 8,000 admissions a year. It’s time to do some renovations. So not only are we making the units nicer, we’ve been able to redesign them in a way that also makes them safer, it makes them more therapeutic. So we are keeping one unit closed, we will renovate it and move units in and then we go to renovate the next one so we are operating 250 beds right now. We are the second largest academic psychiatric hospital in the country and we stay functionally full all the time. What I mean by functionally full is if we have an empty bed, it only means that the patient that has been assigned to that bed hasn’t arrived here yet. Every morning we start the day with a list of anywhere from 30 to 45 patients waiting to come in. Most days we are able to find everyone a bed the same day. We get the same number of discharges in a day, but we stay very busy and functionally full all the time. Houston-Harris County has very, very few civil commitments to the state hospitals anymore, so HCPC essentially fills that role for this area as well.
Kelly: And you mentioned being one of the second largest in the nation with regards to academics so to be clear, who funds HCPC?
Glazier: The majority of the beds and the patient days are funded by the state, out of state general revenue. A smaller portion is funded by the county and then also a small portion are funded – we have a few beds that are available for patients with third-party funding, so another small portion is third-party funding. Most of our funding comes from the Harris Center, through our contract with the Harris Center. We do have one contract that is direct with the county with the juvenile probation department so we have one unit that is set aside specifically for adolescents from the juvenile detention center, but the majority of our funding comes from state general revenue.
Kelly: And with that, what’s probably the biggest challenge that you face here at HCPC in order to really carry out your mission?
Glazier: One of the biggest challenges is trying to do our very best with the beds we have to accommodate all the demand for admissions that we have. We take very seriously our role to try to make sure that patients that are in emergency rooms and in hospitals around the medical center, patients that have been court ordered into treatment, patients that are coming in from the neuropsychiatric center that the Harris Center runs, that when we get requests that we are able to get those patients transported here and admitted as quickly as possible. But trying to balance that with trying to manage the patients and treat the patients that are here as thoroughly as possible is a real challenge; it’s a balancing act. We don’t want to push patients out early just to make a bed for someone else who is waiting. On the same token, I don’t want patients to be waiting inordinately long times in an emergency room or a psychiatric center. So trying to manage that queue, that waiting list, can be a real challenge.
Kelly: And on that exact challenge, taking it to the state-wide level, you’re in a position to be able to look at the way the state of Texas delivers a lot of that care. Do you want to talk a little bit about that position, some of the thoughts you bring with your experience at HCPC to that council?
Glazier: One of the difficulties that we have right now, and it’s worse in certain parts of the state, is there are some patients that need longer term care than just short-term acute care, than just a week. And it’s very difficult sometimes to get a civil commitment to a state hospital where a patient can stay longer and get the treatment they need. That is something that we have to figure out because the lack of those types of beds, not only those but also the lack of residential treatment beds for adults which is another low level of care, the lack of supportive housing beds, the lack of a continuum of beds from longer term acute care to shorter-term acute care to residential to supportive housing is what is causing this constant recidivism of some of our patients and is also part of what is causing this huge number of psychiatric patients who are in the Harris County jail. The Harris County jail is commonly said to be the largest psychiatric institute in the state. In fact, the Harris County jail on any given day has more psychiatric patients that it is housing than in all of the state hospitals combined in the state of Texas. Part of the reason for that is that there are some gaps in our treatment system that if we could fill those, if we had better places that had some treatment of care to discharge someone from HCPC into, and also had sufficient case management services to surround them with, we could eliminate a lot of those recidivists and a lot of those patients who end up in jail.
Kelly: Well, thank you for your time. I know all of you are busy doing so many things so thank you so much for taking some time to be with us.
The Harris County Psychiatric Center has helped thousands of Harris County residents, and yet we know thousands more needs services. Capacity, especially for inpatient mental health services, is a challenge for all of Texans.
There are many issues to be brought up during the interim, and we look forward to hearing more from Chairman Four Price’s Select Committee on Mental Health. We hope this look at capacity has shown how statewide policy must address the ability for those seeking inpatient care to find it, and the consequences of a lack of investment in access.
This is Minding Houston, I’m Bill Kelly.
Music: “Clear Your Head” by Cory Gray and back beats by Frank Nora




 Unfortunately, things haven’t improved since this report was released in 2011. One of the most respected health care groups in Texas just released a report this January that echoes many of the same concerns. In an interview with
Unfortunately, things haven’t improved since this report was released in 2011. One of the most respected health care groups in Texas just released a report this January that echoes many of the same concerns. In an interview with 